Do you experience pain behind your heel ? Does it affect your walking and other activities? If you or loved one experience that then It can be Achilles Tendonitis. Please continue reading to know more about it and how physiotherapy helps with Achilles Tendonitis.
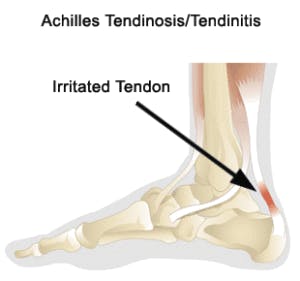
Achilles Tendinopathy is characterised by pain at the back of the heel. The Achilles tendon essentially bears the entire weight of the body in all the weight bearing activities. This makes it prone to a lot of stress and overuse injuries.
There are different types of this condition – midportion (more common) or Insertional.
Insertional Tendonitis involves injury to the portion of the Achilles that inserts into the calcaneus, which is the bone at the heel.
Midportion Tendonitis involves injury to the portion of Achilles a few cm above the insertion.
It is important to distinguish between the two types as the treatment can be slightly different for each type. We are discussing the symptoms, causes and treatment options for the mid-portion Tendonitis as it is more common.
What are the Symptoms?
- The most noticeable symptom is the pain in the Achilles tendon. This pain is usually aggravated on walking, running or any other weight-bearing activities.
- Swelling and thickening of the affected Achilles might be observed as compared to the opposite side
- Stiffness in the Achilles tendon and calf, especially in the morning, is also very common
What are the Causes?
A few common factors that are associated with Achilles Tendonitis are as follow. Your physiotherapist may discuss one or many possible factors that may cause the Achilles tendinitis.
– Poor Footwear
– Flat Feet (Overpronated Feet)
– Overuse : years of running, increased time on foot, any recent change in your activity load (eg. Increase in running time or running distance)
– Calf muscle tightness
– Weak muscles of the calf, hamstring, gluts
– Obesity
– Any direct blow or trauma to the Achilles tendon
Treatment Options –
There is not a consensus about the most optimal treatment option to deal with Achilles Tendinopathy. But evidence shows that exercise is one of the most effective ways to tackle the symptoms associated with midportion Achilles tendonitis. A few things that you can do at home are –
- Ice
If you are experiencing acute symptoms of Achilles pain along with swelling, you can put cold pack at the area to for pain relief and decrease the swelling
- Avoid Walking barefoot or in flat footwear
Use sport shoes to ensure proper foot posture. Orthotics are also very helpful in improving your foot biomechanics.
- Stretching –
Stretching is important to reduce the stiffness in the tendon and the calf muscle. Your Calf is made of 2 different muscles – Gastrocnemius and Soleus. there are different ways to stretch each.
You can use a towel to stretch out as shown below. Hold the stretch for 20 sec and perform 3 times each.
Calf Stretch

2. Common Ankle Strengthening exercises recommended by physiotherapist for Achilles tendinitis.
As mentioned above, exercise has been shown to improve the midportion Achilles tendinopathy. A steady progression of rehab exercises for 6-8 weeks is necessary to completely resolve the symptoms of this condition.
You can begin with some Isometric exercises in the beginning as shown below to start putting load on the muscles of the ankle.
Isometric Ankle muscle strengthening exercises




Further progression can be made to eccentric training exercises. Studies have shown that eccentric loading shows better results in cases of midportion Achilles Tendonitis.
Eccentric Gastrocnemius muscle strengthening exercise


To get a personalised approach to your exercise regime, it is always better to consult an exercise expert to get you through your rehab process.
Remember, if in doubt regarding any aspects of the above options, it is always better to get an opinion by an expert. There are many other treatment techniques that can help you accelerate your healing process. Common Physiotherapy for Achilles tendinitis includes techniques like Shockwave, Laser Therapy, Taping, Massage Therapy, Acupuncture, all have been shown to be effective in adjunct to Exercise Therapy.
Our Heel and foot pain expert at Complete Care Physiotherapy Centre can help you to recover from your heel pain and get you back to your favourite activities as soon as possible. We have successfully treated many heel and ankle injuries in the Etobicoke, Mississauga, Toronto and Vaughan region.